B28. Clinical manifestation of aortic aneurysm. Aneurysma dissecans. Surgical options.
Aortic aneurysm
Aortic aneurysms are diseases of elderly with risk factors for atherosclerosis, like smoking, hypertension, and dyslipidaemia.
We distinguish two types of aortic aneurysms depending on the affected part of the aorta, thoracic aortic aneurysm (TAA) and abdominal aortic aneurysm (AAA). 90% of cases are abdominal. An aortic aneurysm is defined as a dilation > 50% of the normal diameter, or > 3 cm.
Aortic aneurysms are problematic because:
- They can rupture, which kills most of affected people within minutes or hours
- They can cause aortic dissection, which is also highly lethal
- Turbulent flow occurs in the aneurysm, which can cause wall thrombosis with subsequent thromboembolism, potentially causing ischaemic stroke
- They can compress other structures.
These aneurysms typically grow slowly, but the risk of rupture and compression increase with the size.
Etiology
The majority of aortic aneurysms are related to the same risk factors as for atherosclerosis, including hypertension, dyslipidaemia, and smoking. Family history of aortic aneurysm is also a significant risk factor.
However, aneurysms, especially thoracic ones, are rarely associated with inherited connective tissue disorders like Marfan syndrome and Ehlers-Danlos syndrome, as well as giant cell arteritis, Takayasu aortitis, and mycotic aneurysm.
Tertiary syphilis used to be a common cause of aneurysm, but this is much less common nowadays.
Pathology
Degeneration of elastic and collagen fibres, as well as atherosclerosis, causes the formation of the aneurysm. Degeneration occurs due to mechanical stress due to hypertension and due to activation of proteases like collagenase, elastase, matrix metalloproteinase, and plasmin.
Abdominal aortic aneurysm
An abdominal aortic aneurysm is the most common form of aortic aneurysm, the other being thoracic aortic aneurysm. They may be infrarenal (most common) or suprarenal. They usually start below the renal arteries and end above the iliac bifurcation. They can be saccular or fusiform, often with atherosclerotic plaques and large mural thrombi. AAA are usually asymptomatic until they rupture, at which point they are rapidly deadly and have a terrible prognosis. The mortality is 80%, and only 50% ever reach the hospital alive. Anterior ruptures into the abdominal cavity have the highest mortality and rarely reach the hospital alive. Posterior ruptures into the retroperitoneum limits bleeding somewhat, having a lower mortality.
AAA is a disease of elderly men, especially smokers.
It's important to screen for and monitor abdominal aortic aneurysms to reduce the incidence of rupture.
Etiology
See aortic aneurysm.
Clinical features
Non-ruptured abdominal aortic aneurysm (AAA) is asymptomatic. They may be discovered incidentally, during screening, or on routine physical examination as a pulsatile abdominal mass or abdominal bruit.
Ruptured AAA is a different story. Anterior ruptures into the abdominal cavity have the highest mortality and rarely reach the hospital alive. Posterior ruptures into the retroperitoneum limits bleeding somewhat, having a lower mortality. The classical triad involves severe acute abdominal pain, a pulsatile abdominal mass, and haemodynamic instability. A symptomatic AAA is an indication of threatening rupture, including abdominal pain and tender AAA on palaption. Less than 1/3 of patients with rupture have a known history of AAA.
Cullen’s sign (periumbilical ecchymosis) and Grey-Turner sign (flank ecchymosis) are signs of ruptured AAA.
Diagnosis and evaluation
Palpation for a pulsatile abdominal mass is sensitive for normal-weighted people with larger aneurysms, but the larger the person’s abdominal circumference and the smaller the aneurysm, the lower the sensitivity.
Diagnosis is based on imaging which shows an aneurysmal dilation > 50% of the normal diameter, or > 3 cm. Imaging may be achieved with ultrasound or CT.
Treatment
Conservative treatment involves regular surveillance with ultrasound (1 – 3x a year), normalisation of blood pressure, smoking cessation, blood lipid reduction, and removal of other risk factors. This is indicated for asymptomatic AAAs which are < 5,5 cm.
Elective surgery is indicated for aneurysms which are > 5,5 cm, or which expand > 1 cm per year. Emergency surgery is indicated for ruptured AAA. Symptomatic (threatening) AAA must also be treated immediately.
Surgery may be endovascular or open. Endovascular aneurysm repair (EVAR) is preferred. Entry to the aorta is achieved through the femoral or iliac arteries. An expandable stent graft is place inside the lumen of the AAA.
Screening
Many countries have screening programmes for AAAs, screening people above a certain age (usually 50-65) with ultrasound.
Thoracic aortic aneurysm
A thoracic aortic aneurysm (TAA) is the least common form of aortic aneurysm, the other being abdominal aortic aneurysm. This form of aneurysm is located in the thoracic aorta and can affect any segment of it; most frequently, the aortic root and ascending aorta are affected, followed by the descending aorta and the aortic arch. TAA is defined as an increase in diameter by 50% compared to the normal diameter for that segment. Most are asymptomatic, but can rupture or dissect.
Like AAA, TAA is a disease of elderly men, especially smokers.
Etiology
See aortic aneurysm.
Clinical features
Non-ruptured thoracic aortic aneurysm is mostly asymptomatic. They may compress nearby structures and cause chest, back, or flank pain. Compression may also cause hoarseness or lung symptoms. They may be discovered incidentally, during imaging for other conditions.
Aneurysm rupture or impending rupture causes severe pain, hypotension, and shock.
Diagnosis and evaluation
TAAs may be visualised on contrast CT or MRI. Transtorachic (normal) echocardiography can visualise the proximal aorta but not the distal. Transoesophageal echocardiography can visualise the whole aorta. X-rays are rarely used to evaluate a suspected aneurysm, but they may be seen as a convex contour in the mediastinum on chest x-rays taken for other purposes.
Treatment
Conservative treatment involves regular surveillance with ultrasound (1 – 3x a year), normalisation of blood pressure, smoking cessation, blood lipid reduction, and removal of other risk factors. The goal systolic blood pressure should be 105 - 120 mmHg. This is indicated for asymptomatic AAAs which do not fulfill criteria for elective surgery.
The criteria for elective surgical repair of TAA are aortic diameter > 5,5 cm or rapid expansion or elevated aortic size index or aortic area over height ratio. Surgical repair may be achieved with an open or endovascular technique.
Symptomatic and ruptured TAAs are urgent and emergency indications for surgical repair, respectively.
Complications
The risk of aneurysm rupture increases with the size. TAAs between 4-5 cm have <2% yearly risk of rupture or dissection, but TAAs > 6 cm have >7% risk.
Aortic dissection
Aortic dissection refers to the arterial dissection of the aorta and is, like aortic aneurysm, mostly a disease of older men. It’s a quite deadly condition, with high mortality rate even with treatment. It's one form of acute aortic syndrome.
Aortic dissection is problematic because it may rupture the aorta, or it may cause downstream ischaemia. If the dissection occurs above where a branching artery originates, the branching artery will no longer be supplied by blood from the true lumen but rather from the false lumen. Circulation in the false lumen is worse than in the true lumen or even completely absent, which may cause ischaemia of supplied tissues. Thrombi may also form in the false lumen, which may embolise.
Etiology
The biggest risk factors for aortic dissections are:
- Hypertension (70% of patients have it)
- Atherosclerosis
- Connective tissue disease (Marfan syndrome, Ehlers-Danlos syndrome)
- Cocaine use
- Thoracic aortic aneurysm (especially >6 cm)
Classification
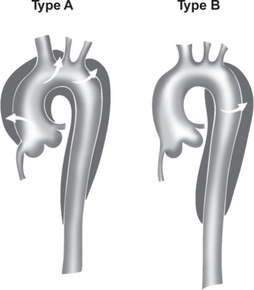
Two classification systems exist for aortic dissections, the Stanford classifications and DeBakey classifications, but the Stanford classification is the one which is used. Stanford type A aortic dissection originates from the ascending aorta and may extend all the way to the iliac bifurcation. Stanford type B aortic dissection originates from the beginning of the descending aorta and may also extend to the bifurcation. Stanford type A is the worst type.
Clinical features
Dissection usually causes sudden severe pain in the chest, back (interscapular), abdomen, or neck. Depending on the complications of the dissection, symptoms of ischaemia of other organs as well as bleeding may also be present:
- Acute myocardial infarction – due to involvement of right coronary artery
- Heart failure, aortic regurgitation – due to involvement of the aortic valve
- Cardiac tamponade – due to involvement of pericardium
- Ischaemic stroke or syncope – due to involvement of carotid or brachiocephalic artery, or due to thromboembolism
- Paraplaegia – due to involvement of spinal/vertebral arteries
- Upper extremity pulselessness, hypotension – due to involvement of subclavian artery
- Mesenteric ischaemia – due to involvement of coeliac or mesenteric arteries
- Haemothorax
- Aortic rupture (see TAA)
There are no specific clinical signs. Involvement of the subclavian artery may cause falsely low blood pressure when measured at the affected arm. Difference in radial pulse and brachial blood pressure between the two arms is relatively specific but only occurs in 30% (if the subclavian artery is affected). Absent pulse in carotid or iliac arteries may be a sign that these arteries are blocked by the false lumen. A diastolic murmur may be audible if aortic regurgitation has occured. Absent bowel sounds may be a sign of intestinal ischaemia.
Diagnosis and evaluation
Chest x-ray may be the initial evaluation and may show widened mediastinum and irregular contour of the aorta.
The gold standard is CT angiography. Visualisation of two lumen separated by an intimal dissection flap gives the diagnosis. The true lumen is often the smaller of the two. The true and false lumen can also be distinguished based on that the great arteries (coeliac trunk, SMA) usually originate from the true lumen. Echocardiography should always be performed to look for cardiac complications.
ECG should always be performed to look for inferior AMI.
Treatment
Aortic dissection is an emergency and so the patient must be admitted, usually to the ICS.
So-called anti-impulse therapy, involving urgent intravenous antihypertensive treatment to decrease BP and HR (which reduces stress on the aortic wall), is always indicated. This involves beta blockers and vasodilators (nitroprusside/nicardipine). The blood pressure should be decreased to lower-normal ranges.
Emergency surgery is indicated for Stanford type A dissections, and Stanford type B dissections with complications. Uncomplicated Stanford type B dissections has lower mortality when treated conservatively rather than with surgery.
Surgery involves the replacement of the affected part of the aorta with a prosthesis, or the insertion of a stent graft, or a combination of the two. An affected aortic valve must be replaced.
Possible procedures include Bentall procedure, Frozen elephant trunk, etc.
For secondary prevention, atherosclerotic risk factors should be treated, and blood pressure should be kept < 140/90.
