18. Pathogenesis of coronary insufficiency. Risk factors
The oxygen delivery to the myocardium can only be increased by increasing the coronary blood flow. If the coronary blood flow can’t be increased to meet the oxygen demand of the myocardium, ischaemia develops.
Coronary circulation
The myocardial metabolism is highly aerobic, meaning that the coronaries must supply a lot of oxygen to the heart muscle. The coronary circulation is 80 mL/100g/min, which is higher than the cerebral blood flow at 60 mL/100g/min. The oxygen extraction from the coronary blood to the myocardium is close to the max, from 10 to 14%. The O2 consumption is 8-15 mL/100g/min.
Because the myocardium already extracts the maximum amount of oxygen from the blood, the oxygen supply to this tissue can not be increased by ways other than increasing the blood flow. This becomes important later.
The subendocardial myocardium of the left ventricle is the unluckiest. During systole the intraventricular pressure is higher than the pressure in the subendocardial arteries, which decreases the blood flow through these arteries. The majority of the perfusion of the subendocardial myocardium therefore occurs during diastole. As a result, the diastolic time is important for the coronary circulation. This puts an upper limit on how high the heart rate can become before the subendocardial myocardium is underperfused.
The coronary blood flow is autoregulated, so that the coronary blood flow stays constant despite large fluctuations in the mean arterial pressure. Coronary blood flow is autoregulated between 60 and 150 mmHg MAP. The small coronary arteries are equipped with β1 adrenergic receptors, which cause vasodilation and therefore increased blood flow.
β1 adrenergic activity, as well as the following factors, increase coronary blood flow:
- Hypoxia
- Adenosine
- K+
- Lactate
- NO
- Prostacyclin
The myocardial oxygen demand increases when heart rate and/or contractility increases. When the myocardium needs to work harder, the coronary circulation must also increase. In healthy hearts the myocardial perfusion demand and coronary supply are equal, so that the myocardium always receives the perfusion it needs.
Coronary insufficiency
When the myocardium has a higher oxygen demand than the coronary circulation can provide, we say that the coronary circulation is insufficient (coronary insufficiency). This causes myocardial ischaemia.
Myocardial ischaemia has many consequences. It is painful, causing the characteristic chest pain called angina, which is involved in ischaemic heart diseases like stable angina and myocardial infarction, as we will see later. Ischaemia decreases the contractility of the ventricles, potentially causing heart failure. It also causes ECG changes which can be used to diagnose it.
Due to how the subendocardial myocardium is only perfused during diastole but the rest of the myocardium is perfused during the whole heart cycle, the subendocardial myocardium is the most suspectible to ischaemia and almost always the first part of the myocardium to become ischaemic or necrotic.
If the ischaemia is severe, the myocardium can become necrotic, in which case acute myocardial infarction occurs.
Factors affecting oxygen demand
Three major points affect the oxygen demand of the myocardium: the heart rate, the contractility and the tension in the ventricular wall. Let’s go through all of them.
The increase in oxygen demand with an increased heart rate is simple to explain. Each beat requires energy. When the heart rate increases will the heart beat more often, increasing the energy and therefore oxygen demand.
Contractility is the measure of force of contraction. When the force of contraction increases will the myocardial cells do more work, meaning that they require more oxygen.
The role of ventricular wall tension in oxygen demand can be hard to understand. When there is tension (stress) on the myocardial wall, myocytes have a harder time contracting and therefore require a higher amount of energy. This means that the myocardium has a higher oxygen demand when the tension increases.
Then, what increases the tension in the ventricular wall? To understand that we must look at the Law of Laplace. This law states that the tension is directly proportional to the pressure inside the ventricle and to the radius of the ventricle but indirectly proportional to the thickness of the wall. The law can be formulated like this:
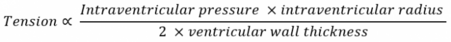
From this law we can derive that an increase in either intraventricular pressure or radius will increase the wall tension and therefore the oxygen demand. Increased ventricular wall thickness however decreases the tension, reducing the oxygen demand.
Three important pathophysiological conclusions can be drawn from this:
- An increase in ventricular wall thickness is beneficial to decrease the myocardial oxygen demand
- Any increase in the diameter of the lumen will increase the wall tension and therefore the oxygen demand
- Any increase in end-diastolic pressure will increase tension and therefore the oxygen demand
Because an increase in ventricular wall thickness decreases the tension and therefore the oxygen demand, the myocardium will respond to increased wall tension by undergoing compensatory hypertrophy, which increases the wall thickness. This initially decreases oxygen demand. However, hypertrophic myocardium requires more oxygen, and as hypertrophy continues the hypertrophic myocardium requires more oxygen than it saves by decreasing the tension. As such, compensatory hypertrophy is not a good compensatory mechanism, as it will eventually increase oxygen demand. Hypertrophic myocardium is also more stiff, which impair diastolic filling.
Several pathologies cause increased oxygen demand by increasing either the heart rate, contractility or wall tension. Here are some:
- Increased afterload
- Systemic hypertension
- Aortic regurgitation or stenosis
- Arrhythmias
- Exercise
Factors affecting oxygen supply
As noted in the beginning of this topic is the myocardial oxygen extraction from the blood close to maximum, even at rest. This means that the oxygen supply can’t be increased by increasing the oxygen extraction, as it is already at its highest level. Oxygen supply can only be increased by increasing the blood flow.
The coronary circulation depends on the difference between the aortic diastolic pressure and the pressure inside the coronary sinus. This difference is called the perfusion pressure. When the perfusion pressure increases will the oxygen supply increase as well.

The coronary reserve is the maximum increase in coronary blood flow that can be achieved by vasodilation (the same concept physiological reserve). It’s essentially how large of an increase in coronary blood flow that can be provided when needed. A large coronary reserve is a good thing, as the coronaries have a large capacity to supply the myocardium with blood even when the myocardial oxygen demand increases.
Coronary reserve is the maximum amount of blood flow that can be achieved minus the blood flow in rest. In healthy persons the coronary reserve is large enough to provide the myocardium with sufficient perfusion in times of increased oxygen demand.
Some factors can decrease the coronary reserve by decreasing the lumen of the coronaries. Atherosclerotic plaques in the coronaries are the most common cause. When the plaques occlude more than 70% of the lumen, ischaemia is so severe that angina pectoris develops.
The smooth muscle in the coronary wall can also spasm, decreasing coronary perfusion. This is characteristic in Prinzmetal’s angina.
Risk factors
The definite biggest risk factor for coronary insufficiency is atherosclerosis. The pathomechanism and risk factors of atherosclerosis are detailed in the pathology 1 topic.
We can collect the risk factors based on how they cause coronary insufficiency:
- Risk factors increasing oxygen demand
- Systemic hypertension
- Aortic regurgitation or stenosis
- Left ventricular hypertrophy
- Risk factors decreasing oxygen supply
- Atherosclerosis
- Anaemia
- Hypoxaemia
- Coronary artery spasm
