13. Molecular mechanisms of blood pressure regulation
The renin-angiotensin-aldosterone system
When juxtaglomerular cells in the kidney sense that arterial pressure is low, they convert prorenin into renin. Renin then converts angiotensinogen secreted by the liver into angiotensin I. Angiotensin I is then converted to angiotensin II in lung capillaries and by endothelial cells by angiotensin converting enzyme. Angiotensin II, which is only 10 amino acids long, is a potent vasoconstrictor and stimulates ADH and aldosterone production, both of which increase blood pressure by conserving fluid.
Angiotensin II binds to angiotensin II receptor type 1 on the vascular smooth muscle cell surface. This receptor activates two separate pathways inside the cell. The first pathway begins with phospholipase C (PLC), which converts PIP2 into IP3, which will bind to its receptor, which will release Ca2+ from the sarcoplasmic reticulum. The second pathway will activate NADPH oxidase, which creates reactive oxygen species like H2O2 (it’s one of the three H2O2 producing enxymes in the body). These species will activate another calcium channel, the L-Type calcium channel, which will cause Ca2+ to enter the cell from outside. Both these pathways increase intracellular [Ca2+], which activates myosin light chain kinase, an enzyme that phosphorylates the light chain of the muscle fibre component myosin. This causes it to contract.
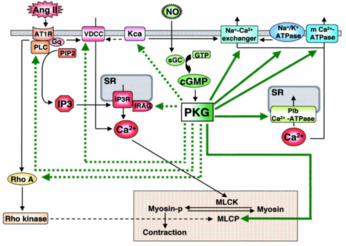
Nitric oxide, a vasodilator, reverses the effects of angiotensin II by decreasing intracellular [Ca2+]. NO activates soluble guanylyl cyclase, which activates PKG. PKG will activate myosin light chain phosphatase, which dephosphorylates the myosin light chain, causing it to decontract. It also activates many Ca2+ channels that let Ca2+ flow back into SR and outside the cell, while inhibiting PLC.
Antihypertensives
Several medications exist to treat high blood pressure. Thiazide diuretics makes your kidneys eliminate more sodium and water, which reduces blood volume, which reduces the blood pressure.
Beta-blockers block the β-adrenergic receptors on the cell surface. They decrease blood pressure by decreasing cardiac output, inhibiting release of renin, and decreasing central vasomotor activity.
Angiotensin-converting enzyme (ACE) inhibitors do exactly what the name say. By inhibiting the formation of angiotensin II, a strong blood pressure increaser, we decrease the BP.
Angiotensin II receptor blockers reduce vascular resistance without reducing cardiac output.
Calcium channel blockers lower blood pressure by inhibiting Ca2+ entry into the vascular smooth muscle cells, which is required for contraction. This causes the smooth muscle to relax, which dilates the vessel.
