4. Inflammatory and ulcerative disorders of the stomach
Written by ms. worldwide, edited by Nikolas.
Many things can go wrong with the GI-tract, and the stomach is not excluded. Let’s look at the pathologies found here.
First, let’s clarify some terms:
- An erosion never goes deeper than the muscularis mucosae, i.e. only the mucosa is affected
- An ulceration goes deeper than the muscularis mucosae, i.e. also the submucosa is affected. It can even perforate the wall.
- A peptic ulcer is an ulcer caused by digestive acid
- Hypochlorhydria is the condition where the level of stomach acid is lower than normal
- Achlorhydria is the condition where there is no stomach acid
Protective and aggressive factors of the gastric mucosa
Introduction
The gastric mucosa is constantly exposed to the stress of gastric acid. There are several factors which are involved in protecting the mucosa against injury due to this stress:
- The mucus layer containing bicarbonate on the surface of the mucosa
- Good mucosal circulation which allows for "washing out" the acid
- Tight junctions between the epithelial cells
- High turnover (regeneration rate) of the epithelial mucosa
- Prostaglandin production which maintain good perfusion, stimulate bicarbonate production, and suppress gastric acid production
- Secretory mucosal IgA
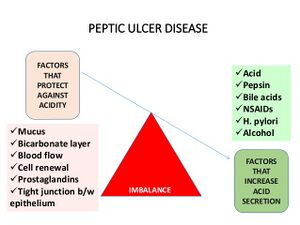
On the other hand, there is a similarly long list of aggressive factors which increase the amount of stress the gastric mucosa is exposed to:
- Secretion of HCl
- Secretion of pepsin
- Helicobacter pylori
- NSAIDs - due their inhibition of prostaglandin synthesis
- Ischaemia and hypoxia
- Smoking
- Alcohol
- Steroids
There is a constant balance between protective and aggressive factors. Should the balance tip towards increased stress, either due to a decrease in protective factors, or due to an increase in aggressive factors, acid-induced injury to the gastric mucosa will occur, including erosions and ulcers.
Helicobacter pylori
Helicobacter pylori is a spiral shaped bacterium which resides in the gastric mucus, adhering to the epithelial cells of the gastric mucosa and causing local inflammation. This bacterium produces the virulence factor urease, which forms ammonia, a base which neutralises the acid around the bacterium, allowing it to survive in the acidic environment of the stomach. However, this urease activity is toxic to the epithelial cells.
H. pylori destroys the somatostatin-producing D-cells in the gastric antrum, leading to decreased somatostatin production, which leads to decreased inhibition of gastrin production, which leads to increased production of gastric acid. This may predispose to the formation of duodenal ulcers.
The inflammation eventually causes atrophy of the local mucous membrane (including the acid-producing parietal cells) and intestinal metaplasia, which predisposes to development of cancer. Inflammation predominantly affects the gastric antrum but may spread to other parts of the stomach if left untreated. Gastric ulcers may also develop due to inflammation and intestinal metaplasia, but in the context of normal or reduced gastric acid secretion.
Inflammatory disorders of the stomach
Acute erosive gastritis
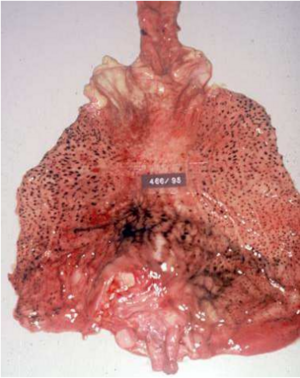
Erosive gastritis refers to the presence of multiple haemorrhagic erosive lesions in the stomach. Often there is minimal or no inflammation present, and so the term gastritis for this condition isn't completely accurate, but the name has stuck in clinical practice. It's also called acute haemorrhagic erosive gastropathy.
Erosive gastritis occurs when the balance of aggressive and protective factors tips in favour of aggressive factors. The most common causes are:
- Heavy use of NSAIDs
- Alcoholism
- Heavy smoking
The erosions frequently bleed, which can cause haematemesis. This bleeding is often self-limiting. Erosive gastritis is a frequent cause of haematemesis in alcoholics.
A (autoimmune) gastritis - Autoimmune metaplastic atrophic gastritis (AMAG)
AMAG occurs in only 1 % of the population, and it is caused by the presence of anti-parietal cell antibodies. 60 % have also anti-intrinsic factor antibodies. Recall that this type of cells is found in the fundus and the corpus of the stomach. AMAG is one of the two causes of atrophic gastritis, the other being H. pylori.
Since the parietal cells have the proton pump, H+/K+ ATPase, these patients suffer from hypochlorhydria or achlorhydria because they lose their parietal cells. If the disease is severe enough, the gastrin levels increase in the serum as well. However, there are usually no symptoms, so the patients slowly develop atrophy of the mucosa in the corpus and fundus. Dyspepsia may develop due to hypochlorhydria.
The parietal cells also secrete intrinsic factor, which is needed to absorb vitamin B12 in the terminal ileum. Therefore, AMAG leads to B12 deficiency, which in this case is called pernicious anemia.
It may also eventually lead to gastric adenocarcinoma or carcinoid tumors.
B (bacterial) gastritis – Helicobacter Pylori associated gastritis
Infection by H. pylori causes H. pylori gastritis, sometimes called B (bacterial) gastritis or environmental metaplastic atrophic gastritis (EMAG). This is a form of chronic atrophic gastritis and present in a whopping 2/3 of the population worldwide. The prevalence is decreasing due to sanitation and antibiotics, but it is still 90% in developing countries. While the infection usually occurs in childhood in developing countries, it usually occurs in adulthood in industrialized countries.
In most cases, the infection is asymptomatic and lasts the whole life. In those that have symptoms can the consequences however be fatal.
- The infection gives a 15-20 % lifetime risk of peptic ulcer disease.
- It has also been linked to 70 % of gastric cancers, especially intestinal types and gastric MALT lymphoma.
- Bacterial toxins, like e.g. cagA, VacA, urease and ammonia are toxic to the epithelial cells
Diagnosis is based on visualisation of the bacterium on biopsy. Treatment involves proton pump inhibitors (PPIs) and antibiotics.
C (chemical) gastritis
This one affects approx. 15 % of the population, and is caused by chemical, toxic or reactive agents which destroys the gastric mucosa. We distinguish between endogenic and exogenic factors.
- Endogenic factors:
- Bile acid or pancreas-fluid reflux
- Exogenic factors
- Alcohol
- Drugs like NSAIDs and steroids
The injuries are almost always found in the antrum and can be seen as foveolar hyperplasia with hyperemia. This type of gastritis is considered mild.
D Gastritis
Here we can find various types of gastritides, which are caused by different factors.
It wasn’t easy to find relevant information for this, so I guess this isn’t that important to know in detail.
- Opportunistic gastritides by cytomegalovirus (CMV) or yeast infection.
- Granulomatous gastritis
- Lymphocytic gastritis
- Collagenous gastritis
- Eosinophilic gastritis
- Gastritis cystica profunda
- Graft vs. host gastritis (GVH-gastritis)
- Allergic gastritis
Peptic ulcer disease
Introduction and etiology
Peptic ulcer disease (PUD) refers to the presence of peptic ulcers in the stomach and/or duodenum. Duodenal ulcers are approx 3 times more common than gastric ulcers. In virtually all cases, patients with PUD either have H. pylori infection and/or use NSAIDs long-term. Few people develop PUD without either of these risk factors.
In addition to H. pylori and NSAIDs, there are multiple other "supportive" risk factors. These include smoking, alcohol, steroid use, and stress. Severe stress like trauma, burns and surgery may predispose to PUD. These ulcers sometimes have special names: Curling-ulcus after severe burn injury, and Cushing-ulcus after CNS injury.
The red factors on the left are the factors that protect against acidity. The green factors on the right are the aggressive factors.
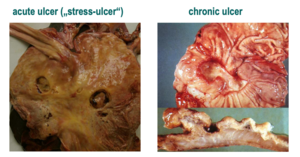
Pathology
The ulcers may occur in any part of the GI-tract that is exposed to acidic gastric juices but is most commonly found in the minor curvature of the stomach, gastric antrum and first portion of duodenum.
We distinguish between acute and chronic ulcers. Let’s take a look at their differences:
| Acute ulcer | Chronic ulcer |
| Mostly smaller than 1 cm | 2 - 4 cm |
| Often multiple | Often just one |
| Round or oval | Radiating mucosal folds around it |
| At the level of the mucosa | |
| Ulcer base: covered by fibrin or hematin | Ulcer base: clear |
| Ulcer edge: grayish, yellow and flat | Ulcer edge: Hyperemic and straight walls |
| Complications: bleeding, perforation, peritonitis | Complications: Bleeding, perforation, penetration, scarring formation |
Complications
Peptic ulcers may bleed, obstruct the gastric outlet, or perforate. Perforation may lead to peritonitis.
Treatment
PUD is treated with proton pump inhibitors, and treating the underlying cause, including avoiding risk factors. Surgery may be necessary if conservative treatment is insufficient.
Zollinger-Ellison syndrome
This syndrome is a rare cause of PUD. It is characterized by multiple peptic ulcerations in the stomach, duodenum and even jejunum. It is caused by neuroendocrine tumors that produce gastrin, called gastrinomas, and they are often located in the pancreas, duodenum or the lymph nodes of the abdomen. Increased gastrin means increased stomach acid.
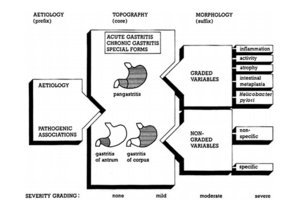
Classification of gastritides – Sydney system
The Sydney system is used to combine the topography, morphology and the etiological information so it’s easier to come up with a diagnosis.
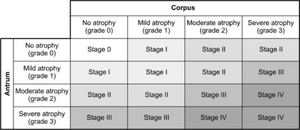
Grading of atrophy – OLGA
The OLGA grading system uses at least five biopsies from five different parts of the stomach to establish which stage the gastritis is in.
Congenital malformations
Fortunately, congenital pathologies of the stomach are rare and not part of the topic for the exam.
- Atresia – complete occlusion of pyloric outlet
- Microgastria – Babies born with abnormal small stomach and limbs
- Duplication – Abnormal growth of a solid tumor or cyst in the GI. Can also appear as bleedings or perforations.
- Gastric diverticulum
All of those above are very rare. Let’s look at some that are still uncommon, but more frequently found than the latter ones.
- Infantile hypertrophic pyloric stenosis – The mucosa of the pylorus is so hypertrophied that it can obstruct the gastric outlet. The infant will therefore projectile vomit after every meal. The mucosa also appears edematous, will have patchy erosions and be full of ulcers. This is not the same as atresia.
- Pancreas heterotopy – This means that the pancreatic tissue can be found outside the pancreas, and in approximately in 1-2 % of the population, it’s found in the stomach.
