32. Passive heterotopy. Causes, forms and consequences
Passive heterotopy refers to the situation when an ectopic focus takes over as the pacemaker and works at a lower frequency than the SA node. These aren’t pathological rhythms but rather compensatory mechanisms and “safety nets” that take over when the SA node cannot conduct signals properly.
There are multiple types of passive heterotopic abnormalities:
- Escape beats
- Escape rhythms
- Junctional escape rhythms
- Ventricular escape rhythms
Etiology
Something prevents the SA node from conducting its signals to the ventricles. The most common causes are:
- 3rd degree SA block
- 2nd degree AV block
- Mobitz type I
- Mobitz type II
- 3rd degree AV block
- Sinus arrest
If the SA node failure or heart block is only brief only a single or a couple of escape beats may occur before the SA node regains control. If the SA node doesn’t soon regain control an escape rhythm occurs.
Complications
The low heart rate of escape rhythms means that the cardiac output is low. The patient can experience symptoms of forward heart failure. Symptoms of cerebral hypoperfusion like fatigue, dizziness and syncope can occur.
If the SA block or AV block occurs suddenly it might take some time for the escape rhythm to kick in. During this time there is asystole and no cardiac output, and the patient can lose consciousness. This is called a Stokes-Adams attack. Stokes-Adams attacks can occur in other cardiac abnormalities as well.
In escape rhythm never kicks in asystole continues and the patient dies.
Escape beat
An escape beat originates from a heterotopic pacemaker, but unlike an extrasystole it occurs later than expected according to the current heart rate.
Escape beats may originate in the junction or the ventricles. Their morphology is similar to that of the escape rhythms.
Junctional escape rhythms
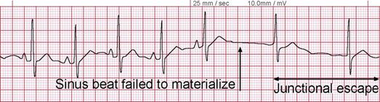
These rhythms originate in the junction between the atria and ventricles, often in parts of the His bundle.
ECG morphology:
- Bradycardia (40 – 60/min)
- P wave
- Can be absent. If present it is negative.
- Can be before the QRS complex – if the pacemaker is in the higher part of the junction
- Can be “inside” the QRS complex – if the pacemaker is in the middle of the junction
- Can be after the QRS complex – if the pacemaker is in the lower part of the junction
- QRS complex is normal
In some cases there can be an accelerated junctional escape rhythm, where the heart rate can be 60 – 100/min.
Ventricular escape rhythms
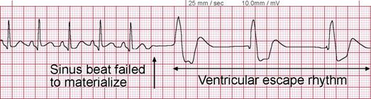
These rhythms originate in the ventricular myocardium.
ECG morphology:
- Bradycardia (20 – 40/min)
- P wave does not precede QRS
- QRS complex is wide
- It might have similar morphology as in LBBB or RBBB
- Secondary ST-segment abnormalities
