7. Alcohol
Summary
- High intake can be toxic to brain, GI tract, pancreas, liver
- Alcohol is absorbed in the mouth, stomach and small intestine
- It is processed by alcohol dehydrogenase/Cytochrome P450/catalase and then by aldehyde dehydrogenase
Not much to write about this
Ingested alcohol is diluted by saliva in the mouth. Some alcohol is absorbed there. After swallowing, more alcohol is absorbed through the stomach, where it irritates the cell lining and increases the acidity of gastric acid. After gastric emptying, the remaining (and most) alcohol is absorbed in the small intestine. Alcohol easily diffuses from the blood into cells, affecting almost every cell in the body. Alcohol can pass the blood-brain barrier. The cells in the brain are not used to toxins, because most of the toxins are stopped by this barrier. Therefore, alcohol has an especially strong effect on the brain. Eventually, the alcohol is metabolized by the liver, and excreted via urine, sweat and exhalation.
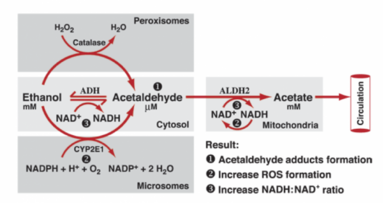
Ethanol is first converted to acetaldehyde and then to acetyl-CoA. The first reaction can be catalyzed by either alcohol dehydrogenase, one of the cytochrome P450 systems (specifically CYP2E1), or by catalase. The first is found in cytosol, the second in ER and the third in the peroxisomes.

The oxidation of ethanol to acetaldehyde and then to acetate reduces NAD+ to NADH, which increases the NADH/NAD+ ratio in the body. This increased ratio is not good, because NADH allosterically inhibits many reactions of the catabolic metabolism, so that less energy is produced. The body therefore tries to reduce the NADH/NAD+ ratio by using lactate dehydrogenase to reduce pyruvate to lactate, which oxidizes NADH to NAD+ in the process. This leads to lactic acid acidosis. However, this also depletes pyruvate, which is an important substrate for gluconeogenesis, so the liver cannot produce glucose for the blood. Therefore, ethanol intake induces both hypoglycemia and lactic acidosis.
The oxidation of ethanol to acetate also produces reactive oxygen species as a byproduct in both the CYP2E1 and aldehyde dehydrogenase reactions, which causes oxidative stress on the body. The end-product, acetyl-CoA, can be converted to fatty acids in the liver. Recall that fatty acid synthesis is activated by high [NADH], which exacerbates this effect. Therefore, overconsumption of alcohol will cause fatty acids to build up in the liver, causing fatty liver disease. Continued exposure to alcohol over a long period of time will lead to increased acetaldehyde levels, which stimulates collagen deposition by the stellate cells in the liver. Byproducts of the liver’s processing of acetaldehyde also damages cell membranes. The sum of these effects will cause the normal liver tissue to be replaced with scar tissue, a condition called cirrhosis.
