19. Systemic and local immunity
The body has both an external and internal surface. The external surface consists of skin and is very large, approximately 1.8 m2. The internal surface however, consists of mucosa and is 400 m2! The skin is a strong physical barrier, which nothing is supposed to leave (except sweat and oils). The mucosa however, must be somewhat permeable to allow the body to take up nutrients from food and oxygen from air. The immune system of the mucosa is therefore more highly specialized than for the skin. We’ll look at them both.
Skin associated immune system (SALT)
Many immune cells are found in the skin. They are Langerhans cells, macrophages, γδ T-cells, αβ (normal) T-cells, B-cells, NK-cells, granulocytes and mast cells. However, another cell type that doesn’t strictly belong to the immune system is quintessential in the SALT. The keratinocytes, the most abundant cell type in the epidermis, produces cytokines and antimicrobial peptides that is stored in the keratin and on the skin surface.
Langerhans cells are specialized dendritic cells located in the skin. After they’ve been activated after phagocytosing something and want to present it to the immune system, they will transform into a cell type called the veiled cell and migrate to a nearby lymph node. Langerhans cells develop from the common myeloid progenitor cell.
Mucosa associated lymphatic tissue (MALT)
Several cell types are important in the MALT. T-cells, MAIT cells (mucosa associated invariant T-cells), NK cells, macrophages, eosinophils, mast cells and granulocytes are all important here.
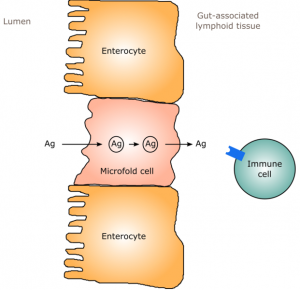
The epithelium of the intestinal mucosa has to be tight with no gaps. However, this also makes it difficult for immune cells to scavenge the gastrointestinal tract for pathogens. Scattered among the epithelial cells of the intestines are so-called M cells (or microfold cells). These M cells can take up antigens from the lumen of the intestine and transport them to APCs which are waiting on the basal side of the M cell. The APCs will then differentiate in the Peyer’s patches of the intestine.
There are three types of tonsils in the oral cavity, the palatine, lingual and pharyngeal tonsils. Pathogens found in the air that we breathe and the food that we eat will meet the lymphatic tissue in these tonsils. Should a pathogen be found there will the body initiate the immune response, which can give it a head start compared to if the immune response started when the pathogen entered the intestines.
As mentioned in topic 13, the IgA isotype is the most important antibody in the defense of the mucosa. There are two subtypes of IgA, IgA1 and IgA2. IgA1 is found in the lamina propria of the intestines, while IgA2 is resistant against the proteases found in the lumen of the gut and is therefore found there.
The mucosal surfaces of the body are interconnected in a secretory immune system. If a pathogen is found in the intestine and presented to APCs an immune reaction will occur that ends with antibodies produced against the pathogen in all the mucosal surfaces in the body, and not just where the infection happened. IgA antibodies will then be found in the saliva, tears, the urogenital system, the respiratory tract and the lactating breast.
