14. The structure, function and origin of erythrocytes
Red blood cells

RBCs are small cells in the blood. They’re red, which is why the blood is red as well. RBCs are 7 – 8 µm in diameter, and they have a biconcave disc shape, which is difficult to explain but easier to show.
The shape is important because it allows the cells to be flexible. The RBCs must squeeze through very small vessels called capillaries, which may be around 5 – 10 µm in diameter themselves, so it’s important for them to be flexible. You shouldn’t think of RBCs as solid cells but more like bags of haemoglobin, that can easily fold and squeeze through small capillaries.
RBCs don’t have nuclei, so they don’t have DNA and therefore can’t make any more proteins or replicate. They don’t have mitochondria, so they can’t produce energy by oxidative phosphorylation and must produce energy by anaerobic glycolysis.
They also contain an enzyme called carbonic anhydrase, which is very important for pH buffering and for transport of CO2.
Haemoglobin
The red colour of RBCs comes from the fact that they contain a lot of haemoglobin (Hb). Haemoglobin is a protein that contains an iron ion. In adults it’s comprised of four globin units (two α and two β) plus one heme group. It is the heme group which contains the iron (Fe2+) ion. Each molecule of haemoglobin can bind up to 4 molecules of oxygen (O2).
The function of haemoglobin is to carry oxygen in the blood. 1 gram of Hb can bind 1.39 mL of O2 gas. 99,7% of oxygen in the blood is transported via haemoglobin; only 0,3% of oxygen is dissolved in the blood.
There is a lot of haemoglobin in each RBC, so that 35% of the RBCs size comes just from haemoglobin. This is important, because if the body has problems synthesizing enough haemoglobin the RBCs will be smaller than normal (less than 7 µm).
The normal value of haemoglobin in the blood is 140 – 160 g/L. There is no free haemoglobin floating around in the plasma – all haemoglobin in the blood is inside RBCs. Normal RBC count in the blood is 5.0 – 5.5 million/µL in males and 4.5 – 5.0 million/µL in women.
More about haemoglobin is described in topic 17.
Anaemia is the condition where the blood contains too little haemoglobin. This is often caused by the blood containing too few RBCs (erythropaenia), or if there is a normal number of RBCs but they contain less-than-normal haemoglobin. Erythropaenia literally means “low number of erythrocytes”. It can be caused by:
- Haemorrhagic (bleeding) anaemia – if a person is bleeding will they lose both blood cells and blood plasma. The body can quickly replenish the plasma that was lost; however it takes 3-6 weeks to replenish the lost blood cells, especially the RBCs. During this time there is more plasma than RBCs and there is therefore anaemia.
- Aplastic anaemia is a condition where the bone marrow isn’t functioning properly, meaning that it can’t produce the normal number of RBCs.
- Haemolytic anaemia – haemolysis means “destruction of RBCs”. If RBCs are continuously destroyed by the body will the number of RBCs obviously be low.
- Iron deficiency anaemia – the body needs iron to produce haemoglobin. See below for details.
- Folate or B12 deficiency anaemia – the body also needs folate and B12 to produce RBCs. See below for details.
Erythrocytosis is the condition where the number of RBC is elevated above normal. This may not seem like a problem at first but can be dangerous because more RBCs in the blood makes the blood more viscous (thicker), which increases blood pressure. Erythrocytosis can occur if there is a cancer-like growth in the bone marrow that produces RBCs uncontrollably. This condition is called polycythaemia vera. It can also occur if the level of oxygen in the blood is low so that the body tries to compensate by producing more RBCs, which is called polyglobulia.
Synthesis
RBCs are produced in the bone marrow and released into the circulation, where they live for around 120 days. The rate of production of RBCs is controlled by the kidney. The kidney produces a hormone called erythropoietin, or EPO for short. When the kidney produces more EPO, it is a signal to the bone marrow that it should produce more RBCs.
What influences the kidney’s EPO production? RBCs carry oxygen in the blood. When there is little oxygen in the blood (hypoxaemia) the kidney will receive less oxygen (hypoxia) and respond by producing more EPO, which causes more RBCs to be produced. More RBCs in the blood may compensate for the low amount of oxygen in the blood.
The synthesis of RBCs in the bone marrow require some important compounds. We divide them into two groups – those compounds that are necessary for the synthesis of haemoglobin and those that are necessary for the synthesis of the cell itself:
- Necessary for haemoglobin production:
- Iron (Fe2+)
- Necessary for RBC production
- Folic acid (or vitamin B9 or folate)
- Vitamin B12
If you have too little iron in your body the bone marrow won’t have enough iron to produce enough haemoglobin. This means that each RBC produced will contain smaller-than-normal amounts of haemoglobin, which also makes the RBC itself smaller than normal, a condition called microcytosis, or microcytic anaemia.
Vitamin B12 and folic acid are important for synthesis of the cell itself and not haemoglobin. If you have too little of either of these two will the body be unable to produce as many RBCs as it wants to. To try to compensate for this will the body fill each RBC with more haemoglobin, so that each RBC becomes larger than normal. This condition is called macrocytosis, or macrocytic anaemia.
Pernicious anaemia is a type of B12 deficiency anaemia where the stomach doesn’t produce enough intrinsic factor (IF). Intrinsic factor is a protein produced by the stomach which is essential for the gastrointestinal tract to absorb vitamin B12. When the stomach can’t produce IF the body can’t absorb vitamin B12 from food, so B12 deficiency occurs.
RBC parameters
Haematocrit is the volume percentage of RBCs to the blood, i.e. how many percent of the total blood volume is taken up by RBCs. I mentioned above that the cellular elements comprise around 45% of the total blood volume. There are so many RBCs compared to the other cell types, so only the RBCs determine the haematocrit.
The normal value of haematocrit is 0.44 – 0.46 (44% – 46%) in males and 0.42 – 0.44 (42% – 44%) in females.
Because the RBCs make up virtually all of the haematocrit will changes in the haematocrit mostly indicate changes in the number and sizes of RBCs. Haematocrit is low (lower than 0.44 or 0.42) when there are too few RBCs (erythropaenia). The haematocrit is high in erythrocytosis or when the plasma volume is decreased, such as in dehydration.
Measuring the mean RBC size can be important in determining whether there is microcytosis or macrocytosis. This is done by taking a blood sample, measuring the diameter of the RBCs and plotting it into a curve. This curve is called a Price-Jones curve, and in healthy people will almost all RBCs be around 7-8 µm, so there will be a peak there.
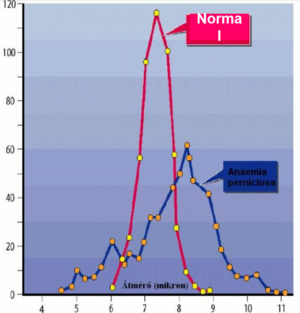
If the peak is lower, i.e. below 7 µm there is microcytosis, which indicates iron deficiency anaemia. If the peak is higher, i.e. above 8 µm there is macrocytosis, which indicates B12 or folate deficiency anaemia.
The average volume of each red blood cell is called mean corpuscular volume (MCV). Its normal value is 80-95 fL. The f stands for femto-, which is one billionth of a µL. This value is elevated in macrocytosis and decreased in microcytosis. MCV can be calculated like this: MCV = haematocrit / RBC count.
The average amount of haemoglobin in each RBC is called mean corpuscular haemoglobin (MCH). Its normal value is 26-36 pg (picogram). A picogram is one millionth of a microgram (µg). The value is increased in macrocytosis, which occurs in B12 and folate deficiency. When there isn’t enough B12 or folate the bone marrow can’t produce enough RBCs, so it will pack the RBCs it can produce with more haemoglobin to compensate. MCH is decreased in microcytosis, when the body can’t produce enough haemoglobin, which occurs in iron deficiency. MCH can be calculated like this: MCH = total mass of haemoglobin in blood / RBC count.
The average concentration of haemoglobin in each RBC is called mean corpuscular haemoglobin concentration (MCHC). Its normal value is 310 – 360 g/L blood and it is calculated like this: MCHC = total mass of haemoglobin in blood / haematocrit.
Reticulocytes
Reticulocytes are immature RBCs in the blood. They circulate for about a day before developing into mature RBCs.
Unlike mature RBCs reticulocytes have endoplasmic reticulum and ribosomes. This means that they still have the capability of protein synthesis, unlike RBCs.
The number of reticulocytes reflects the degree of erythropoiesis. When there are more reticulocytes in the blood than normal the bone marrow is producing more RBCs than normal and vice versa. The number of reticulocytes is usually represented as a percentage of all RBCs.
Normally, 0,5 – 1,5% of RBCs in the blood are reticulocytes. If this number is decreased it reflects insufficient erythropoiesis, for example due to aplastic anaemia. If it is increased it reflects increased erythropoiesis, often due to blood loss or haemolytic anaemia.
Degradation of erythrocytes and haemoglobin
RBCs are degraded in a part of the immune system called the reticuloendothelial system (RES) or the mononuclear phagocyte system (MPS). More specifically they’re destroyed mostly in the spleen. The rest of the degradation is described in topic 7.
