B18. Malignant tumors of the stomach: Difference between revisions
(Created page with "{{:Gastric cancer}} = Gastrectomy = {{:Gastrectomy}} Category:Surgery final (POTE course)") |
No edit summary |
||
| Line 1: | Line 1: | ||
{{:Gastric cancer}} | {{#lst:Gastric cancer|surgery}} | ||
= Gastrectomy = | = Gastrectomy = | ||
{{:Gastrectomy}} | {{:Gastrectomy}} | ||
[[Category:Surgery final (POTE course)]] | [[Category:Surgery final (POTE course)]] | ||
Latest revision as of 16:24, 28 July 2024
Gastric adenocarcinoma accounts for 95% of gastric cancers. It’s a cancer of elderly, mostly men, and it’s the fifth most common cancer worldwide. It is more common in Asian countries like Japan and Korea, as well as certain regions in Africa and South America.
It causes no or only nonspecific symptoms in the early stages. If diagnosed early, the prognosis is excellent, but at the time of diagnosis, 50-75% of cancers have already spread and are incurable, which leads to a poor prognosis overall.
The mortality of this cancer is higher in the countries with low prevalence because screening is not performed as often as in high-prevalence countries. Therefore, the cancer is often discovered too late.
Other types of gastric cancer are described at the end of the article.
Etiology
- H. pylori gastritis or other atrophic gastritis
- Diet rich in nitrates or salts
- Alcohol
- Nicotine use
- Epstein-Barr virus
- Gastric adenomas
- Previous partial gastric resection
Plant-based diet is protective against gastric cancer.
Pathology and classifications
95% of cases of gastric cancer are adenocarcinomas. The carcinoma is usually located in the antrum, followed by corpus and fundus.
We distinguish “early” and “advanced” gastric cancer. Per definition, “early” gastric cancer infiltrates no deeper than the submucosa but even early cancer can give metastasis to the lymph nodes, while “advanced” cancers infiltrate the muscularis propria and deeper.
Metastatic spread
Gastric adenocarcinoma often spreads to skeleton, liver, lung, brain, and the peritoneum. The Virchow lymph node, the left supraclavicular lymph node, is the most common site of gastric cancer metastasis.
Diffuse type of gastric adenocarcinoma may metastasise to both ovaries (bilateral), forming a so-called Krukenberg tumour.
Clinical features
The stomach is large and spacious, meaning that the tumour may grow large before symptoms appear. Early symptoms of gastric cancer include dyspepsia and mild epigastric discomfort or pain. Later, symptoms like anorexia, early satiety, weight loss, anaemia, and nausea/vomiting.
Diagnosis and evaluation
Physical examination may reveal a tumour in the epigastrium, and an enlarged Virchow’s node (left supraclavicular lymph node). DRE may reveal positive Blumer sign. Faecal occult blood tests may be positive if the tumour is bleeding.
Upper endoscopy is the investigation of choice, as it allows for both visualisation and biopsy. After the diagnosis, CT thorax and abdomen are necessary for staging.
If peritoneal carcinosis is suspected but not visible on imaging, laparoscopy may be necessary to visualise the peritoneum and diagnose the carcinosis. Cytology may be obtained from the ascitic fluid. Molecular diagnosis is important to detect any overexpression of HER2, VEGF, or PD-L1 which is important in case of advanced cancer.
Treatment
Stages I – III are curable, with metastatic (stage IV) gastric cancer usually being incurable. Cancers located only in the mucosa or submucosa (“early” gastric cancer) may be treated endoscopically or with minimally invasive surgery.
Surgery
The standard curative surgical treatment for “advanced” gastric cancer patients is radical gastric resection with lymphadenectomy. For intestinal type gastric cancer, distal or subtotal gastric resection is performed. For diffuse type gastric cancer, total gastrectomy is necessary. Afterwards, the GI system must be reconstructed by Roux-en-Y, Billroth I, or Billroth II.
Surgery may be used palliatively as well, in cases where the tumour obstructs passage of foodstuffs, for example. A stent may be placed, the stomach may be resected, or bypass surgery may be employed.
Gastrectomy
Gastrectomy refers to the surgical resection of the stomach. To maintain gastrointestinal function, gastrectomy must be followed by a form of reconstruction surgery, most commonly Roux-en-Y.
Indications
- Gastric cancer
- Severe, complicated peptic ulcer disease
- Weight loss (obesity)
Types
Partial gastrectomy (also called distal or subtotal gastrectomy) refers to resection of only the distal part of the stomach. It may be used for gastric cancers in the distal 2/3rds of the stomach, when adjacent lymph nodes are also removed.
Total gastrectomy (also called radical gastrectomy) refers to complete removal of the whole stomach. It may be used for gastric cancers localised in the proximal stomach.
Sleeve gastrectomy refers to removal of 80% of the stomach, along the greater curvature. This decreases the size of the lumen, promoting satiety.
Reconstruction surgeries
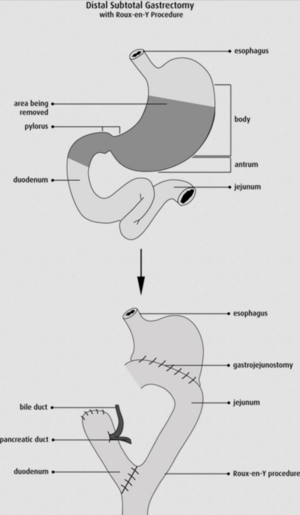
The Roux-en-Y reconstruction surgery is the most frequently performed reconstructive surgery of the proximal GI tract, as it prevents bile reflux. The stomach is separated from the bile-containing duodenum by a strand of jejunum 50 cm long. It is difficult to explain how this works, so I’ll allow this image to do the explaining.
Billroth
Billroth I refers to the procedure where the distalmost part of the stomach is resected, and an anastomosis is formed between the duodenum and the remaining distalmost part of the stomach in an end-to-end fashion. This can only be performed if the cancer is located distally in the stomach, close to the pylorus. This procedure is rarely performed anymore, and never in the surgical unit of POTE.
Billroth II refers to the procedure where a larger resection of the stomach is performed, and an anastomosis is formed between the side of the duodenum and the side of the remaining stomach in a side-to-side fashion. This procedure allows for a larger resection of the stomach than Billroth I. However, Billroth II allows bile to reflux into the stomach, which causes metaplasia and cancer progression in the remaining stomach or oesophagus. As such, Billroth II is rarely performed anymore, and never in the surgical unit of POTE.
Complications
Many complications may occur after gastric resection:
- Post-gastrectomy gastritis
- Stoma stenosis
- Dumping syndrome
- Maldigestion
- B12 deficiency
