35. Polypus adenomatosus coli (p53)
Staining: Immunohistochemistry targeting the protein p53
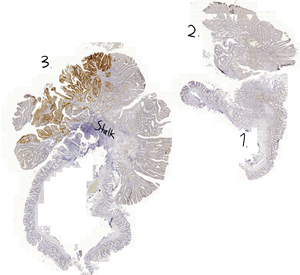
Organ: Colon
Description: Three sections can be seen. We’ll call the lower right section for section 1. Here we can see colonic crypts, and no villi. Goblet cells are present. Section 2 is the section above. Here we can see that the crypts contain bubble-like structures. No goblets cells are present.
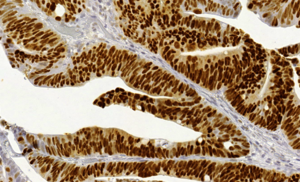
The interesting part about section 3 is the epithelium that is stained brown. The staining is inside the nuclei and not in the cytosol of the stained cells. Also notice that the stalk in section 3. Otherwise is it similar to section 2.
Diagnosis: Adenomatous polyp in the colon

Risk factors:
- Western diet
- Inflammatory bowel disease
Theory:
Immunohistochemistry (IHC) staining works (in simple words) by producing an antibody with a colour attached to it. When the antibody binds to something the colour will be visible. The antibody in this case binds to the protein p53, a tumor suppressor protein. Dysregulation of p53 is closely related to the development of colorectal cancer.
Colonic polyps are classified in three ways:
- According to their macroscopy (sessile/pedunculated)
- According to their microscopical features (tubular/villous/tubulovillous)
- Whether dysplasia is present or not (hyperplastic/adenomatous)
Polyps that look like mushrooms growing out of the mucosa are called pedunculated polyps. They have stalks that separate them from the colonic mucosa. Polyps that don’t have stalks and instead diffusely grow out of the mucosa are called sessile polyps. Pedunculated polyps are easier to remove, due to their stalk. Polyps that have the tubular structures seen in this slide are called tubular polyps. Polyps can also have villi on their surface, then they’re called villous polyps. Polyps with both villi and tubular structure are called tubulovillous polyps.
Lastly, if there’s no dysplasia in the polyp is it a hyperplastic polyp, which does not increase the risk for cancer. However, if there is dysplasia is it an adenomatous polyp, which does increase the risk for cancer.
Section 1 is of from a healthy part of the colon. No p53-positivity is seen. It has crypts and goblet cells.
Section 2 is from a fragment of a polyp, but this fragment isn’t p53 positive either. The bubble-looking structures are tubular structures, showing that this is a tubular type of polyp and not a villous one (although it could have been tubulovillous, but no villi are seen in this case). The polyp contains no goblet cells, because the polyp is only made up of dysplastic epithelium.
Section 3 is a cross-section of a polyp with intestinal mucosa. A part of the polyp is positive for p53. It’s important to note that the nuclei of the cells are p53-positive, not the whole cell.
With IHC staining it’s impossible to determine whether there is dysplasia or not. During routine biopsy of a polyp is both an IHC and a HE slide made. The HE slide is used to determine whether there is dysplasia, and the IHC slide is made to determine whether the polyp is p53 positive. However, even in this slide can we be certain that there is dysplasia, because p53 positivity cannot occur in polyps where there is no dysplasia.
The p53 positivity shows that in this polyp has p53 already been mutated. This means that this patient has increased risk for colorectal cancer (but doesn’t have cancer yet).
To summarize: The polyp in this slide is a tubular, pedunculated, adenomatous polyp that is p53 positive.