Acute coronary syndrome: Difference between revisions
No edit summary |
No edit summary |
(No difference)
| |
Latest revision as of 14:15, 28 April 2024
Acute coronary syndrome (ACS) is an umbrella term for acute presentations of coronary artery disease or ischaemic heart disease. ACS is used as an initial working diagnosis for coronary-type chest pain until an ECG and troponin level has been performed, which will decide which type of ACS the patient has.
There are three types, each of which with differing underlying pathophysiology:
- Non-ST elevation coronary syndrome (NSTE-ACS)
- Unstable angina (UA)/unstable angina pectoris (UAP)
- Non-ST elevation myocardial infarction (NSTEMI)
- ST elevation myocardial infarction (STEMI)
STEMI and NSTEMI are both types of acute myocardial infarction (AMI). According to the fourth universal definition of myocardial infarction it is defined as "clinical evidence of acute myocardial ischaemia and with detection of a rise and/or fall of cardiac troponin".
Initial evaluation
After insuring that the patient is ABC stable, the patient should undergo ECG and a blood test to measure for troponin levels. STEMI needs acute, urgent management, while NSTE-ACS needs a risk stratification before deciding the timing of management. High risk patients with NSTE-ACS should be treated acutely like STEMI, while low risk patients can be treated on a longer timescale. For this reason, it’s important to determine the type of ACS early, and if it’s either of the NSTE-ACS’s, perform a risk stratification.
The results from the ECG and troponin test will give the working diagnosis:
- ST-elevations are present in two consecutive ECG leads corresponding to a part of the heart supplied by a specific vessel -> the diagnosis is STEMI
- ST-elevations are not present in ECG leads corresponding to one part of the heart -> the diagnosis is NSTE-ACS
- Troponins are elevated and are dynamic -> the diagnosis is NSTEMI
- Troponins are not elevated -> the diagnosis is unstable angina or the cause is not coronary
Troponins
Troponins are proteins located in striated muscle. Two forms of troponin, cardiac troponin I (cTnI) and cardiac troponin T (cTnT) are only found in cardiac muscle and are used in the diagnosis of acute myocardial infarction. When the myocardium becomes necrotic cTnI and cTnT are released into the blood, which can be measured.
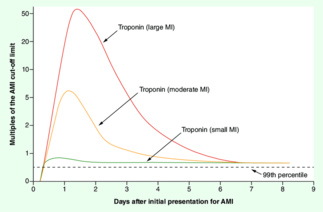
In both forms of myocardial infarction (STEMI and NSTEMI), the troponin levels increase as the damage is ongoing, peak when the injury has passed, and then start to decrease. For this reason, if you measure the troponin level at 2 different times when there is an AMI, the troponin level is going to be higher or lower at the second measurement, depending on whether the troponin peak had been reached or not at the time of the first measurement. This is called a rise and/or fall in troponin and is often referred to as troponin dynamics. Many conditions can cause troponin elevation, but troponin dynamics are highly specific for AMI. As such, if the diagnosis of AMI is not immediately certain, a repeat troponin measurement should be taken after 1 – 3 hours, and if a rise and/or fall is present, the diagnosis is certain. A significant rise and/or fall is defined as a change of > 20 – 50%.
However, the magnitude of troponin elevation corresponds to the myocardial damage. While conditions like heart failure and myocarditis also can cause troponin elevation, they virtually never cause a very large elevation in troponins. if the troponin levels are very high (even if only measured once), the risk for AMI is sufficiently high that we may proceed to invasive management without waiting for a repeat troponin. Modern high-sensitivity troponin assays have an upper normal limit of normal of approx. 14 ng/L. As the single-measurement troponin increases beyond 1000 ng/L the specificity for AMI increases.
Modern high-sensitivity troponin assays can detect a rise in troponins 1 – 3 hours after the infarction. As such, the troponins may be normal if measured early. In these cases, a repeat measurement should be performed 1 – 3 hours later.
Other biomarkers of myocardial injury
Other biomarkers of myocardial injury exist. Creatine kinase-MB is an isoform of creatine kinase which is mostly (but not exclusively) found in myocardium. CK-MB has a shorter half-life than troponins and may therefore be used to detect small re-infarctions better than troponins.
Myoglobin is not exclusively found in myocardium and is therefore not specific to myocardial injury. It has a very short half-life. It's rarely used in the diagnosis of myocardial infarction.
Ischaemia-modified albumin was researched as a biomarker of myocardial injury, and it bore promise as it increased within minutes of infarction, but it is not specific enough for myocardial injury to be useful.
Echocardiography
An echocardiography should also be performed in the emergency department. Regional hypokinesis or akinesis in regions corresponding to the blood supply territory of one coronary artery increases the likelihood that there is AMI. In addition, echocardiography may reveal alternative diagnoses, like aortic dissection, pericardial effusion, aortic stenosis, hypertrophic cardiomyopathy, or right ventricular dilation suggestive of acute PE.
Rhythm monitoring
All patients with suspicion for ACS should have their heart rhythm continuously monitored with a rhythm monitor. The risk for fatal arrhythmias is highest in the first days after an AMI.
