Aortic dissection: Difference between revisions
(Created page with "'''Arterial dissection''' occurs when there defect in the arterial tunica intima, leading to blood entering a virtual space between the tunica intima and tunica media. This forms a so-called ''false lumen'' inside this space. Unlike what the image at the top of the page shows, the false lumen may become larger than the true lumen. Blood may flow out of the false lumen through a second intimal tear. The aorta is the artery most often affected by dissection. Aortic dissec...") |
(No difference)
|
Revision as of 14:31, 16 November 2023
Arterial dissection occurs when there defect in the arterial tunica intima, leading to blood entering a virtual space between the tunica intima and tunica media. This forms a so-called false lumen inside this space. Unlike what the image at the top of the page shows, the false lumen may become larger than the true lumen. Blood may flow out of the false lumen through a second intimal tear.
The aorta is the artery most often affected by dissection. Aortic dissection is, like aortic aneurysm, mostly a disease of older men. It’s a quite deadly condition, with high mortality rate even with treatment.
Aortic dissection is problematic because it may rupture the aorta, or it may cause downstream ischaemia. If the dissection occurs above where a branching artery originates, the branching artery will no longer be supplied by blood from the true lumen but rather from the false lumen. Circulation in the false lumen is worse than in the true lumen or even completely absent, which may cause ischaemia of supplied tissues. Thrombi may also form in the false lumen, which may embolise.
Etiology
The biggest risk factors for aortic dissections are:
- Hypertension (70% of patients have it)
- Atherosclerosis
- Connective tissue disease (Marfan syndrome, Ehlers-Danlos syndrome)
- Cocaine use
- Thoracic aortic aneurysm (especially >6 cm)
Classification
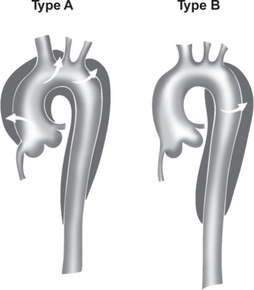
Two classification systems exist for aortic dissections, the Stanford classifications and DeBakey classifications, but the Stanford classification is the one which is used. Stanford type A aortic dissection originates from the ascending aorta and may extend all the way to the iliac bifurcation. Stanford type B aortic dissection originates from the beginning of the descending aorta and may also extend to the bifurcation. Stanford type A is the worst type.
Clinical features
Rupture usually causes sudden severe pain in the chest, back (interscapular), abdomen, or neck. Depending on the complications of the dissection, symptoms of ischaemia of other organs as well as bleeding may also be present:
- Acute myocardial infarction – due to involvement of right coronary artery
- Heart failure, aortic regurgitation – due to involvement of the aortic valve
- Cardiac tamponade – due to involvement of pericardium
- Ischaemic stroke or syncope – due to involvement of carotid or brachiocephalic artery, or due to thromboembolism
- Paraplaegia – due to involvement of spinal/vertebral arteries
- Upper extremity pulselessness, hypotension – due to involvement of subclavian artery
- Mesenteric ischaemia – due to involvement of coeliac or mesenteric arteries
- Haemothorax
- Aortic rupture (see TAA)
There are no specific clinical signs. Involvement of the subclavian artery may cause falsely low blood pressure when measured at the affected arm. Difference in radial pulse and brachial blood pressure between the two arms is relatively specific but only occurs in 30% (if the subclavian artery is affected). Absent pulse in carotid or iliac arteries may be a sign that these arteries are blocked by the false lumen. A diastolic murmur may be audible if aortic regurgitation has occured. Absent bowel sounds may be a sign of intestinal ischaemia.
Diagnosis and evaluation
Chest x-ray may be the initial evaluation and may show widened mediastinum and it may be normal.
The gold standard is CT angiography. Visualisation of two lumen or an intimal dissection flap gives the diagnosis. Echocardiography should always be performed to look for cardiac complications.
ECG should always be performed to look for inferior AMI.
Treatment
Aortic dissection is an emergency and so the patient must be admitted.
So-called anti-impulse therapy, involving urgent intravenous antihypertensive treatment to decrease BP and HR (which reduces stress on the aortic wall), is always indicated. This involves beta blockers and vasodilators (nitroprusside/nicardipine). The blood pressure should remain < 140/90 for life. Atherosclerotic risk factors should be treated.
Emergency surgery is indicated for Stanford type A dissections, and Stanford type B dissections with complications. Uncomplicated Stanford type B dissections has lower mortality when treated conservatively rather than with surgery.
Surgery involves the replacement of the affected part of the aorta with a prosthesis, or the insertion of a stent graft, or a combination of the two. An affected aortic valve must be replaced.
Possible procedures include Bentall procedure, Frozen elephant trunk, etc.
