23. Antiarrhythmic drugs: Difference between revisions
(Created page with "== Cardiac electrophysiology == We can divide the normal action potential into 5 phases: # Upstroke phase # Early-fast repolarization # Plateau # Repolarization # Diastole thumb|This shows the action potential of the ventricle. The phases are marked with numbers. These phases can be seen on the figure below. Note that this shows the depolarization of the ventricle. The cardiac pacemaker cells don’t have “normal” act...") |
(No difference)
|
Revision as of 14:50, 16 March 2023
Cardiac electrophysiology
We can divide the normal action potential into 5 phases:
- Upstroke phase
- Early-fast repolarization
- Plateau
- Repolarization
- Diastole
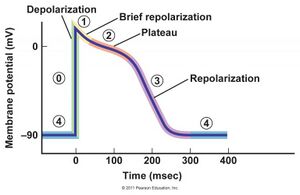
These phases can be seen on the figure below. Note that this shows the depolarization of the ventricle.
The cardiac pacemaker cells don’t have “normal” action potentials, so they skip phase 1 and 2. In these cells is phase 0 the rapid depolarization, phase 3 the repolarization and phase 4 the spontaneous diastolic depolarization.
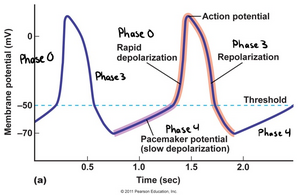
The figure above shows how the cardiac pacemaker cells in the sinus node and AV node spontaneously depolarize. The membrane slowly depolarizes by itself (phase 4) until it reaches the threshold, at which point the membrane spontaneously depolarizes (phase 0). After this will the membrane repolarize (phase 3) The period of slow depolarization on the figure is called the spontaneous diastolic depolarization (SDD). From the figure can you see that the minimal membrane potential, the lowest membrane potential reached during SDD, is around -70mV.
There are four different “phenomena” that lie in the background of arrhythmias:
- Increased automaticity
- Spontaneous action potentials in myocardial cells
- Premature depolarization
- Re-entry
- AV block
Introduction to antiarrhythmic drugs
This type of drug is used to prevent recurrent arrhythmias and to restore sinus rhythm in people with current cardiac arrhythmias. Antiarrhythmic drugs are classically classified according to the Vaughan Williams classification. There are four drug classes in this classification:
- Class I – Na+ channel blockers
- Class Ia – Intermediate Na+ channel blockers
- Class Ib – Weak Na+ channel blockers
- Class Ic – Strong Na+ channel blockers
- Class II – Beta blockers
- Class III – K+ channel blockers
- Class IV – Ca2+ channel blockers
Some antiarrhythmic drugs don’t fit into this classification and are mentioned outside it.
Cardiac electrophysiology is a difficult thing. By treating one problem can we produce another. While these drugs are antiarrhythmic, the reality is that they only work in specific situations – antiarrhythmics that in some situations decrease arrhythmia may be pro-arrhythmic in other situations or even in the same situation. This is a severe issue and limits their clinical use.
Some classes of antiarrhythmics are more proarrhythmic than others. From most to least pro-arrhythmic, these are Ic > Ia > Ib > III > IV > II. Class IV and class II antiarrhythmics have virtually no proarrhythmic potential and are therefore the most frequently used.
Note also that studies have shown that the use of antiarrhythmics in non-life-threatening arrhythmias does not decrease mortality and may even increase it. All antiarrhythmics are associated with severe side-effects, primarily due to their proarrhythmic effect.
Another classification, the Sicilian Gambit, classifies the drug based on their effects drugs on ion channels, receptors, pumps considering their clinical and ECG actions. It’s much more complicated and not very relevant to know.
Class I antiarrhythmics
Compounds
Three types of class I drugs exist: Class Ia, Ib and Ic. The different types affect the action potential in different ways.
- Class Ia – Intermediate Na+ channel blockers
- Quinidine
- (Disopyramide)
- (Procainamide)
- Class Ib – Weak Na+ channel blockers
- Lidocaine
- (Mexilitine)
- Class Ic – Strong Na+ channel blockers
- Propafenone
- (Flecainide)
Class Ia drugs, mexilitine, and flecainide are rarely, if ever, used. Lidocaine is a local anaesthetic as well, and it’s much more often used as that than as an antiarrhythmic.
Mechanism of action
These drugs are Na+ channel blockers. These channels are responsible for the phase 0 of the ventricular action potential and phase 4 of the pacemaker action potential. Blocking these channels causes the rate of depolarization during phase 0 to decrease.
Class Ib drugs have a stronger effect on ischaemic myocardium than healthy myocardium, theoretically making them a good choice for arrhythmias that occur after AMI.
Side effects
Class Ia drugs prolong the QT-interval, which increases the risk for torsade de pointes. Class Ic drugs are especially proarrhythmic in case of ischaemia and so is contraindicated in ischaemic heart disease.
Quinidine causes cinchonism, a condition characterised by symptoms like headache, hearing/vision loss, tinnitus, and psychosis.
Class II drugs – beta blockers
Compounds
For more details, see the topic on adrenergic receptor antagonists.
The class II drugs are beta blockers. These drugs prevent sympathetic activity-triggered arrhythmias. They have the no pro-arrhythmic effect.
For the use as antiarrhythmic are β1 selective beta blockers with no intrinsic sympathomimetic activity (ISA) preferred.
Indications
Beta blockers are widely used in cardiology. Their major antiarrhythmic use lies in preventing the occurance of sudden cardiac death due to ventricular fibrillation after myocardial infarction, but they are also used in atrial fibrillation, paroxysmal supraventricular tachycardia and premature ventricular beats.
Class III antiarrhythmics
Compounds
- Amiodarone
- Dronedarone
- Sotalol
The class III drugs are K+ channel blockers. The most important drugs here are amiodarone. Amiodarone is the only used antiarrhythmic drug without a negative inotropic effect, which makes it widely used. It’s therefore the only antiarrhythmic drug (except beta blockers) which can be used in heart failure.
Dronedarone was developed which is an amiodarone analogue without the iodine-atom, which would hopefully be equal in efficacy to amiodarone but without its side effects. However, it turned out that dronedarone is both less effective and more hepatotoxic than amiodarone, and it has therefore not replaced amiodarone.
Like the name suggests, sotalol is also a beta blocker, but it has strong K+ channel blocking activity and is therefore classified as a class III antiarrhythmic.
Indications
- Atrial fibrillation
- Ventricular arrhythmias
Mechanism of action
The class III drugs are K+ channel blockers. These channels are responsible for repolarization. Amiodarone also blocks Na+ and Ca2+ channels and α and β adrenergic receptors.
Side effects
For all of them:
- QT prolongation
Amiodarone is famous for its various side effects, which are important to learn:
- Corneal deposits
- Photosensitivity of the skin with bluish discoloration
- Thyroid dysfunction (as amiodarone contains iodine atoms)
- Pulmonary fibrosis
For side effects of sotalol, see the side effects of beta blockers.
Pharmacokinetics
Amiodarone is very lipophilic, which causes it to slowly accumulate in adipose and other tissues, giving it a very long half-life of 1 month.
Class IV antiarrhythmics – calcium channel blockers
Compounds
- Verapamil
- Diltiazem
These drugs are Ca2+ channel blockers. This channel is important for the phase 0 in pacemaker cells. These drugs have very little proarrhythmic effect. For more details, see the topic on calcium channel blockers.
Indications
- Atrial fibrillation
- Paroxysmal supraventricular tachycardia
Other antiarrhythmics (class V)
As stated earlier are there some drugs that can be used antiarrhythmically but aren’t included in the original Vaughan Williams classification. In newer forms of the Vaughan Williams classification, they’re called class V drugs.
The most important ones are digoxin, adenosine, magnesium sulphate and vernakalant.
Indications
Digoxin may be used for rate control in atrial fibrillation and in heart failure.
Adenosine is used to terminate paroxysmal supraventricular tachycardias.
Magnesium sulphate is used to terminate torsade de pointes. Due to its membrane-stabilizing properties, it is often used as an adjunct in other arrhythmias as well.
Vernakalant is used to convert atrial fibrillation to sinus rhythm.
Mechanism of action
Adenosine binds to A1 adenosine receptors which cause a negative dromotropic effect.
Magnesium stabilizes the membrane potential.
Vernakalant blocks multiple ion channels in the atrial myocardium, making it atrial-specific.
Side effects
Adenosine can cause bronchospasm and hypotension.
Therapy
When patients present with arrhythmias, elimination of provoking factors of the arrhythmia should be the primary objective. Myocardial hypoxia, stress, smoking, electrolyte disturbances are all factors that can provoke arrhythmias and that can be treated. Treating the provoking factor may cause the arrhythmia to fix itself or not reoccur.
It is also important to keep in mind that not all arrhythmias need medical therapy, especially if the medical therapy carries more risk than just leaving the arrhythmia. Many arrhythmias don’t need to be corrected.
